Healthcare systems currently face a funding crisis, which is adversely affecting health outcomes. High unemployment and the slow pace of recovery have further weakened the public sector and its ability to supply quality health services in Europe. This trend is spreading beyond Europe to other geographies, including the US, as economies across the globe are far more interdependent than ever before. The current financial crisis is an acute form of what is likely to become chronic in many western economies. The scale of the challenge not only requires solutions that are effective in the short term, but also some bold and radical measures in the medium to long term.
OVERVIEW
The economic downturn and the consequent squeeze on public spending have significantly affected spending on healthcare in Europe and North America. Despite signs of recovery, the economic environment remains fragile, with a strong possibility that some countries may implement further austerity measures to stabilize their finances. This, in turn, is expected to significantly affect publicly funded healthcare systems.
In many countries, healthcare is likely to enter a period of extended austerity. Further, the pressures that are surfacing are likely to be a common feature of many health systems in future.
The unfunded entitlement payments (burden of social security, Medicare and other entitlements in excess of money set aside for them) may be as high as 188 percent of GDP, in the US. The National Health Service (NHS) in England has a task to become 20 percent more productive by 2015. Other healthcare systems have already started buckling under the pressures of increasing demand and constricted public finance.
The demographic imbalance caused by an increase in aging population globally leads to a much larger issue of change in dependency ratio — reduced tax-paying and working population to support the retired population and those using healthcare services. This imbalance is leading to a growing demand for healthcare globally.
Demand-side pressures — such as an increase in chronic diseases and the number of patients with multiple conditions — are significant challenges to the way healthcare systems operate. However, the majority of growth in health expenditure over the last 20 years has been driven by policy choices and supply-side factors. In fact, factors such as increasing use of technology; new drugs; improved facilities that help provide services to an increasing number of patients; rising costs of providers; and the tendency for spending on healthcare to grow at more than 0.5–2.5 percent above GDP growth have generally had a greater impact on health expenditure than aging has. Its likely that up to one-third of the growth in public health expenditure could be modified by policy decisions.
Countries, states and payors will need to adopt new and more sustainable approaches to service delivery and healthcare funding. In the long-term, many health systems may face the challenge of containing the impact of population changes while simultaneously managing expectations, saying no to developments and reprioritizing existing expenditure.
In the US, the emergence of both the Patient Protection and Affordable Care Act (PPACA) and accountable care organizations (ACOs) reflects a realization of the need to contain spending. Even so, the ambition to slow the rate of increase in expenditure suggests that the urgency of the situation may not have been fully reflected in the legislation. In Europe, while many short-term measures exist to contain costs and review the extent of coverage, there are no signs yet of providers, payers or policymakers having identified alternative models that are likely to be financially sustainable in the long term.
RISING HEALTHCARE EXPENDITURE
Over the past few years, total healthcare expenditure has risen in both developed and emerging markets. Public spending on health constitutes a significant share of total government expenditure and GDP. In most cases, health expenditure has increased, often more rapidly than GDP. During times of recession, the widening gap is also likely to be reinforced by a decrease in GDP growth rates.
According to OECD estimates, public health expenditure as a percentage of GDP is likely to increase by an average of 3 percent in advanced economies, over the next 20 years. This growth is higher than the growth in the 28 years up to 2008 (i.e., between 1980 and 2008), during which time only six countries had growth in excess of 2.5 percent, while some grew at a significantly lower rate — six had less than 1.5 percent growth over this period.
The situation in the US is especially worrisome, as public health spending as a percentage of GDP is projected to rise by about 5 percent over the next 20 years. Medicare spending is expected to continue its upward trend and is projected to grow faster than the GDP. According to estimates by the Congressional Budget Office (CBO), Medicare spending amounted to US$572 billion in 2011, and is expected to be more than US$1 trillion in 2021.6 Moreover, according to the 2011 Medicare Trustees Report, unfunded Medicare benefits to its beneficiaries are likely to total approximately US$24 trillion over the next 75 years.7, 8 The reforms introduced under the Patient Protection and Affordable Care Act (PPACA) of 2010 are expected to expand health insurance coverage and reduce the budget deficit. However, forecast savings on healthcare spending are not very high and the future of these reforms remains uncertain.
On the other hand, in Europe, public health expenditure is expected to increase at an average rate of 2 percent of the GDP, and by more than 3 percent in seven European countries, over 2011–21. Although the current health budget cuts are expected to reduce healthcare spending in the short term, the long-term impact remains uncertain.
In emerging economies, public health expenditure is projected to rise by 1 percent of the GDP over the next 20 years, representing one-third of advanced economies’ total projected growth. The challenges related to public health spending are also different for these economies. In these economies, health coverage is less extensive than in advanced economies, allowing a better scope to increase healthcare spending.
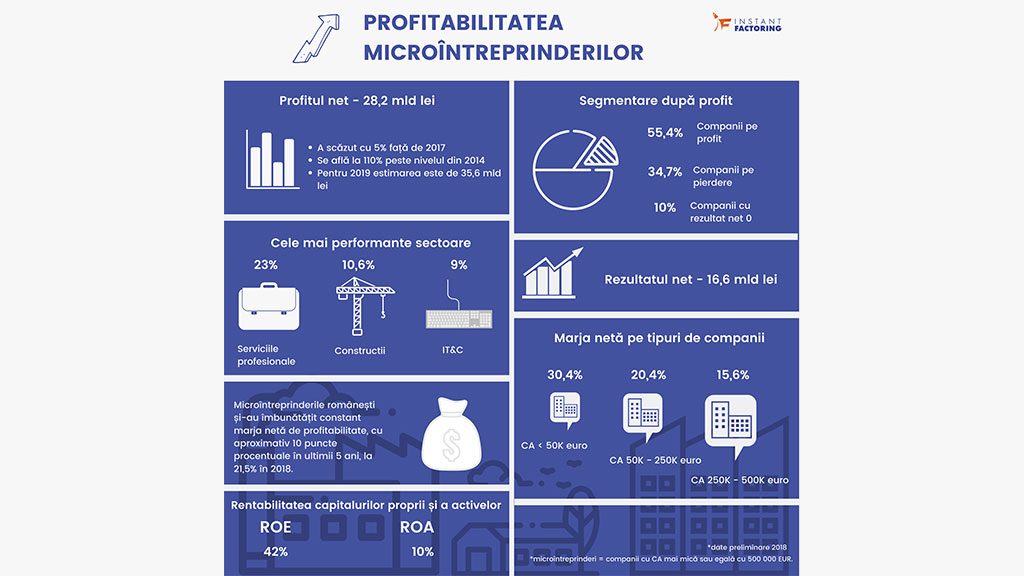
In Romania, total health expenditure, public and private has decreased over the last years from 5.6% of GDP in 2009 to 3.7% in 2011. According to Cegedim, the pharmaceutical market in Romania is forecasted to increase by around 8.9% in local currency in 2012 as compared to previous year and by 6% in local currency in 2013, but remains highly volatile to the market uncertainties.
CONTAINING EXPENDITURE
Lack of additional funding sources will compel policymakers to squeeze the costs of providers and change the way the money is spent. Spending methods can be altered by:
• Reducing benefits offered to the population by implementing measures such as completely removing some items from coverage; increasing patient wait times; substituting generic for branded medication; and implementing health technology assessment systems
• Requiring patients to cover a proportion of the cost by introducing or increasing cost sharing
• Reducing the size of the population covered, for example, by mandating high earners to take private insurance
However, all these methods have risks. If not properly designed, they can lead to patients failing to seek early treatment and increase health inequalities. In fact, approaches such as reducing benefits — particularly by removing high-income groups from coverage — have the potential to undermine the solidarity principle that underpins all successful social insurance and tax-based systems. Adding to this, the implementation of such measures may be extremely difficult from a political standpoint.
BUDGETS FOR FY 2013
Many national governments have recently announced their budgets for FY13. Most countries are either freezing or cutting spending.
For example, in April 2012, the Spanish government announced cuts to health and education spending of EUR10 billion (US$13 billion) per year. It also approved Royal Decree-Law 16/2012, which outlines a series of measures to contain public health expenditure, such as increasing medicine copayments and establishing a new central purchasing system for prescription drugs and health technology assessment systems.
The US budget for FY13 proposes applying a premium surcharge for new beneficiaries, beginning in 2017, if they choose Medigap coverage. It also introduces new TRICARE copayments and fees, to help limit the cost of healthcare while maintaining quality.
The UK government announced public spending cuts of up to GBP2 billion (US$3.3 billion), to fund reduction in income tax for more than 20 million people.
The Canadian government outlined cuts to the healthcare budget proposed in March 2012. Over the next four years, the government plans to reduce the increases in healthcare budget it allocates to various provinces.
While measures taken to control the supply-side costs of healthcare — such as restraining payments, freezing capital investments, controlling prices, closing hospitals and reducing providers’ budgets — seem effective in the short term, they tend to be counter-productive and ineffective in the medium to long term. The scale of the challenge that faces many healthcare providers is such that it now requires a more radical redesign of internal processes as well as the way personnel work. It also requires bold rethinking around the way services function, the role of hospitals and business models, which, in many cases, have remained unchanged for decades.
REGIONAL RESPONSES: EUROPE
Current healthcare scenarios
Healthcare systems are organized and financed in different ways across Europe. Health insurance coverage is either universal or almost universal in all European Union (EU) member states, through compulsory social health insurance or national/local health service provision. Public expenditure accounts for a high proportion of total expenditure (77 percent in 2008). However, the share of private healthcare insurance is increasing. Copayment and direct spending accounts for a small share of total healthcare expenditure (14 percent in 2008 — EU average). To ensure access to services by vulnerable groups, such as low-income individuals and patients suffering from chronic diseases, a system of cost-sharing exemptions is applied in almost all countries.
The healthcare sector across the continent is facing the heat of the ongoing debt crisis and is struggling to balance budgets and restrain spending. Other trends have further exacerbated the financial crisis:
• Changing demographics — aging population and rise in chronic diseases
• Rising cost of healthcare — for example, rising cost of medical technology
• Increasing patient awareness of their entitlements
• Unhealthy lifestyles
• Financing structures and policies aligned more toward providing acute rather than chronic care
Governments' response
Health expenditure accounts for a significant and growing proportion of resources in Europe. Almost all European countries are adopting measures to contain healthcare spending, allocate available resources adequately and manage expenditure on health and hospital care effectively and efficiently. These include the direct rationing and control of expenditure, price cuts; changes in the extent of coverage and cost sharing; reference pricing for reimbursement; policies related to generic medicines; and the reorganization of the decision-making process, such as through the adoption of health technology assessment (HTA).
1. Rationalization of healthcare budgets, staff and services:
Most EU member states have adopted extremely direct cost-containment measures — reducing their healthcare budgets, headcount and services. For example, Romania reduced its health budget by a quarter and also reduced the number of employed healthcare professionals' and workers’ salaries by a similar fraction in 2010.
Countries such as Cyprus, Portugal and the UK introduced hiring and/or salary freezes, while others, such as Hungary, the Republic of Ireland and the Baltic Republics, made salary cuts. Luxembourg passed a legislation that allows the government to cap the number of health professionals over the next five years. In Latvia, the number of medical institutions providing inpatient healthcare was reduced from 59 in September 2009 to 42 in January 2010.
2. Increase in cost sharing:
The increased cost sharing/copayment of medicines, lower reimbursement rates, and a rise in prescription fees are some of the methods that governments are using to reduce public healthcare expenditure. This has helped raise funds for the sector as well as reduce the demand for healthcare goods and services (mostly pharmaceuticals, dental care and eye glasses). Given the current situation of fiscal constraints and in view of demand pressures, cost sharing is likely to be used more extensively over time. However, its application to the entire population and its ability to create substantial revenues are under debate.
In the past two years, countries such as Iceland, Latvia, Denmark and Portugal have either introduced or increased copayments for certain products. As a part of the Social Security Budget Bill, the Economic Committee on Health Products (CEPS) in France changed the reimbursement rate of drugs with "moderate clinical benefit" from 35 to 30 percent and for drugs with "low clinical benefit" from 20 to 15 percent. In Luxembourg, patients’ contribution toward the payment of certain medical and paramedical services has been increased. Out-of-pocket expenditure on hospital stays has risen from an average of EUR12.9 (US$17.2) to EUR19.4 (US$25.7). Patients’ contribution of 12 percent toward nursing care has also been introduced in the country.
In Spain, based on the recently announced budget cuts, employed people will have to contribute more to the cost of medicines, with copayments rising from the current 40 percent to 50–60 percent, depending on the patient's income level. Patients earning an annual salary higher than EUR100,000 (US$132,360) will contribute to 60 percent of the cost, which will be capped at EUR 60 (US$79) a month.
3. Reduction in drug prices and coverage:
Countries such as Germany, Greece, Spain, Ireland, Denmark, Sweden, France and the UK have adopted measures such as price cuts or freezes to reduce expenditure on medicine. Most price cuts have been in the range of 4–5 percent. France also intends to curtail tax incentives for orphan drugs. Greece has designed a program to save more than US$2.5 billion, by reducing drug prices by at least 20 percent.
Additional changes have been introduced to reimbursement lists in many countries. Drug reimbursements in France were reduced from 35 percent to 30 percent in 2010. Iceland introduced changes in reimbursement status on specific group of medicines such as antidepressants.
Comparative Effectiveness Research (CER), conducted by health technology assessment (HTA) agencies such as the National Institute for Health and Clinical Excellence (NICE), is increasingly being employed for drug coverage and pricing decisions in Europe. Countries such as England, Denmark and Sweden have adopted different approaches to using CER in drug coverage decisions. HTA agencies help establish a well-documented and comprehensive overview of the consequences of new healthcare technology. With new expensive technologies additionally burdening healthcare agencies in the times of crisis, HTA can help assess the cost-effectiveness of such technologies and tackle the cost burden more effectively.
An EUnetHTA project has also been initiated to create an integrated, effective and sustainable network for HTA across Europe. To tackle the complexity of pricing and reimbursement across Europe, the concept of an integrated, Europe-wide, reimbursement agency ‘EuroNICE’ is also being discussed.
4. Policies for managing pharmaceutical expenditure:
A number of policies such as generic promotion; financial incentives such as discounts, rebates, clawbacks and paybacks; external price referencing; mark-ups; and value-added tax (VAT) on medicines are directed at pharmaceuticals and pharmacists.
- Promotion of generics: International non-proprietary name (INN) prescribing and generics substitution are two key measures used to promote the use of generics. INN prescribing is mandatory in Estonia, Lithuania, Portugal and Romania. In Denmark, Germany, Finland, Malta, Sweden and Slovakia, pharmacists are obliged to apply generic substitution. In other EU countries, pharmacists may substitute an equivalent, less expensive product — for example, a generic or parallel imported product — for a prescribed medicine. In 2011, Belgium and Latvia introduced new rules for pricing generics in a cluster. Drugs are grouped in clusters and a reference price is set for all drugs within a cluster.
- Reference price system (RPS): The RPS prices drugs by reference to therapeutic comparators, including generic drugs. In 2010, Estonia included 50 percent of all reimbursable medicines in the RPS and implemented new rules for pricing generics and biologics via this system.
- Increase in VAT: VAT on medicines has been increased in several countries. Greece raised its VAT twice during 2010, before reducing it in 2011.
- Distribution margins: Changes in drug payment schemes have affected wholesale and pharmacies in the distribution chain. Wholesale markups have been reduced in Greece, Latvia and Italy. Despite the crisis, pharmacy margins have also been increased in a few countries, including Spain, Portugal and Italy. Pharmacy markups have also been reduced in Switzerland.
- External price referencing (EPR): EPR compares the prices of medicines in one country to those in others to arrive at a pricing and/or reimbursement decision. Malta and Germany have introduced this pricing procedure (under specific circumstances, only applicable from 2012), while four other European countries have modified their existing EPR system — they have extended their basket of reference countries and changed the methodology for calculation to obtain a decreased price.
- Other discounts, rebates, clawbacks and paybacks: Spain introduced discounts of 7.5 percent on original products and 4 percent on orphan medicines in March 2010.
Introduced in Romania in 2009, the clawback system was revised several times. The system obliges pharmaceutical companies to pay back any expenditure on pharmaceutical reimbursement in excess of the amount approved in the budget (on quarterly basis). Payments are due from companies on the basis of their market share. The system has faced criticism from Romania’s pharmaceuticals industry, one of the reasons being the increased level, sometimes exceeding the imposed margin for certain prescribed medicines. Also, the pharmaceutical players have to pay the tax applicable to sales that they will collect after 300-360 days. It is projected that the value of the Romanian pharmaceuticals market (from a producer’s perspective) will decline nearly 30 percent, as a result of the clawback system.
In Poland, a new Reimbursement Law Reform was enforced on January, 2012, introducing an obligatory payback system under which the applicant receiving a reimbursement decision will have to pay back an ‘excess amount’ (calculated by a set formula) to the National Health Fund, whenever the reimbursement budget (i.e.17 percent of the public funds assigned to finance guaranteed healthcare benefits) is exceeded.
5. Fiscal support:
To mitigate the impact of the economic crisis on government budgets, sector spending and household income, the World Bank is providing fiscal support to a number of European countries (Hungary, Latvia, Poland, and Romania) in the area of healthcare reforms. The loan programs include technical assistance and policy dialog for reforms.
6. Health promotion and disease prevention:
Improving health can be an effective way to prevent or control potential increases in healthcare expenditure. Unhealthy lifestyles, obesity and habits such as alcohol consumption and smoking can have a significant adverse impact on health in future. Many countries in Europe are therefore stressing the need to promote health and wellness to reduce the burden of disease and manage healthcare demand more effectively. Countries such as Greece have raised taxes on alcohol and tobacco to discourage excessive use.
Health systems’ response
In the UK, hospitals plan to improve efficiency by at least 5 percent annually, for the next four years, and a national program has been launched to improve efficiency and productivity and sustain quality. The NHS has a task to become up to 20 percent more productive by 2015.
Health systems are adopting measures and policies to reduce the demand for public healthcare products and services. One way is to discourage use of such services, for example, by changing the perception of people toward access to these services. This has indirectly given impetus to private healthcare services and has also increased the share of private expenditure in these services.
1. Increased waiting times:
The focus on cost reduction is leading to an increase in the number of people in waiting lists at many healthcare organizations. The number of patients who are choosing to pay for their own care, after having their treatment delayed or denied altogether, is also growing. The Estonian Health Insurance Fund faced a similar situation in March 2009, when it had to extend the maximum waiting period for outpatient specialist visits from four to six weeks.
2. Relocation of services:
A number of services from walk-in centers in the UK are being integrated within hospital trusts or other local urgent care services, as a step to deliver better health outcomes for the patients. For example, a walk-in center in Tooting in South London was incorporated into the accident and emergency (A&E) department at a nearby hospital (St. George’s hospital).
3. Restructuring of hospital system and services:
Emphasis on primary and outpatient specialist care and homecare is growing, in a bid to reduce the unnecessary use of hospital care and to improve the efficiency, effectiveness and responsiveness of health systems. The use of a ‘referral system’ has been implemented by a number of EU member states, in which a general physician (GP) or a primary care physician is the first point of contact and serves as a gatekeeper/care coordinator to other types of care (specialist outpatient care or hospital care).
The Portuguese healthcare system is going through a number of changes to improve the continuity of care. Portugal aims to achieve efficiency in healthcare through the restructuring of its primary care network (health centers/family health units) and secondary care network (hospitals) as well as the development of the integrated care network. The Mobile Support Unit for homecare offers support to patients with chronic diseases, who are dependent on technology. These units help decrease hospital admissions and associated costs, as well as improve people's quality of life.
Focus on the provision of medical care services at home in Latvia is also growing. Medical care services at home are provided if outpatient treatment is required on a regular basis but the patient is unable to attend a healthcare institution to receive this care for reasons such as being too chronically ill or being immobile following surgery or trauma. There are about 189 centers for homecare in Latvia.
Germany provides incentives for care coordination through its 'disease management programs,’ which include financial incentives for service providers and for sickness funds to focus on the treatment of the chronically ill.
Greece, on the other hand, is an example of a country plagued by inefficiency in primary care. Specialist physicians are in oversupply, while GPs and nurses are in short supply. Lack of a functional referral system and coordination between public and private providers has further compounded the problem. This has led to high healthcare costs and inadequate access to healthcare in the country. The country is working toward improving interaction between GPs and doctors, enhancing the use of medical records and strengthening the role of homecare and community care.
Romania’s health system is also confronting with numerous problems, such as underfunding, lack of transparency and inefficiency in funds allocation, instability within the political and regulatory system and shortage of well qualified health personnel. Romania’s public health system is currently financed, mainly, through compulsory social insurance based on the principle of solidarity, which is collected to the state budget.
Although the private healthcare sector has grown over the last years in Romania, following the massive investments made by the private healthcare providers, the private health expenditure is still very low.
The new healthcare law, which is currently under debate, aims to generate savings to the state budget and to increase the efficiency of resources used, based on a public-private insurance system and hospitals reorganization. It provides, among others, the revision of the package of basic services to cover spending that patients cannot afford. The cheap services will be supported by the patients, while the money saved will be used for serious illnesses. The contributors will have the possibility of selecting the insurance company and the medical services supplier and could also voluntary opt for an additional insurance for services not covered by the basic package.
Implications for other sectors related to healthcare system
The eurozone crisis is increasing pressure on sectors related to the healthcare industry such as life sciences companies, insurance providers, outsourcing companies and procurement companies.
Pharmaceuticals:
According to the European Federation of Pharmaceutical Industries and Associations (EFPIA), unpaid debts owed to the pharmaceuticals sector are estimated up to US$16–20 billion.
Greece, Portugal, Spain and Italy are major contributors to total unpaid bills in Europe. According to Spanish industry group Farmaindustria, at the end of December 2011, Spain’s national health system owed pharmaceutical companies EUR6.37 billion (US$8.7 billion), a year-on-year growth of 36 percent.
The average delay in making payments in Spain is now 525 days, with four Spanish regions exceeding the 800-day mark. These delays are compounding the burden on the pharmaceuticals industry, which is struggling with challenges of patent losses, high research and development (R&D) costs and increasingly stringent regulatory compliance requirements.
In Romania, payment terms exceed in practice 300 days.
In February 2012, Greece introduced a plan to cut drug spending by US$1.3 billion.70 The implementation of price cuts imposed on pharmaceutical companies to reduce expenditure on medicines has had a considerable effect on the financial performance of many companies. Price cuts and mandatory discounts levied by Greece, Ireland, Italy, Portugal and Spain have cost drug companies more than EUR7 billion (USD 9.5 billion) in 2010 and 2011.
According to EFPIA, the state-controlled price cuts in countries such as Greece and Romania have also led to shortages of some medicines, due to parallel trade. This has weakened the aggregate growth for the top five European pharmaceutical markets, which collectively grew 2–3 percent in 2011. Pharmaceutical companies have implemented certain remedial measures such as offering cash on delivery, switching from hospitals to pharmacies and supplying relatively old and inexpensive versions of drugs.
In the last years, lower prices in Romania generated an increase in parallel trade, reaching in 2011 to 298 applications and to 414 applications in the first six months of 2012, according to the representatives of National Agency for Medicines and Medical Devices. According to Cegedim, parallel trade is estimated to reach EUR 700 million in 2012, as compared to EUR 500 million in 2011.
Outsourcing:
In the wake of restrictions on healthcare spending, pharmaceutical companies are increasingly turning to emerging markets to outsource manufacturing and other functions such as R&D to achieve growth and improve margins. According to a report by Frost & Sullivan, the European Pharmaceutical and Biotech Contract Manufacturing Markets, the European pharmaceutical contract manufacturing market is expected to grow substantially from US$10.02 billion in 2011 to US$20.75 billion in 2018. During the same period, the European market for biotechnology outsourcing is forecast to grow from US$1.21 billion to US$2.67 billion. Local contract research and manufacturing services companies in emerging markets such as India, Brazil and China are also likely to gain a number of partnership opportunities.
Procurement:
In many countries, cuts in wholesale and pharmacy margins are likely to impact the distribution and procurement of pharmaceutical products.
IMPACT ON HEALTH
Fiscal austerity programs aiming to reduce public spending on healthcare may have a negative impact on overall public health. Although some austerity measures may have been designed to reduce costs while not affecting the quality of care, they pose a risk of negatively affecting health outcomes or status of a population. For example, while cost sharing or charging patients for specific services could reduce the unnecessary use of services, it may also reduce the necessary use of services by vulnerabl